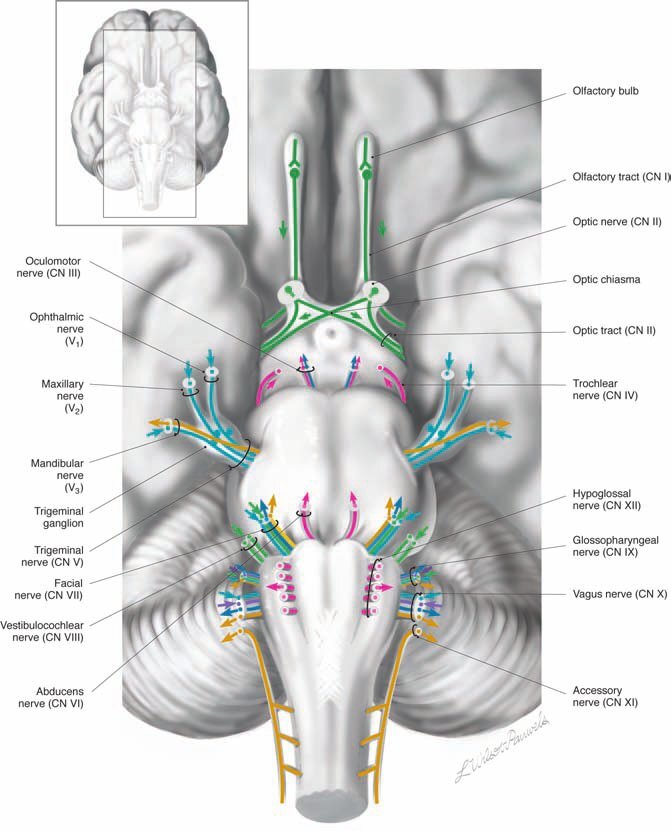
Cranial nerves
The twelve pairs of cranial nerves provide sensory and motor innervation for the head and neck including general, visceral, and special sensory; and voluntary somatic, branchial, and involuntary parasympathetic motor control. Because these nerves emerge from the cranium, they are called cranial nerves, as opposed to spinal nerves that emerge from the spinal column.
The cranial nerves function as modified spinal nerves. As a group, they have both sensory and motor components; however, individual nerves may be purely sensory, purely motor, or mixed (both motor and sensory). The cranial nerves carry six distinct modalities - three sensory and three motor.
These modalities are:
General sensory nerves, which mediate touch, pain, temperature, pressure, vibration, and proprioceptive sensation;
Visceral sensory nerves, which mediate sensory input, except pain, from the viscera;
Special sensory nerves, which mediate smell, vision, taste, hearing, and balance;
Somatic motor nerves, which innervate the voluntary muscles that develop from the somites;
Branchial motor nerves, which innervate the voluntary muscles that develop from the branchial arches;
Parasympathetic (visceral) motor nerves, which innervate the viscera, including glands, bodies, mucosae, and all involuntary smooth muscle.
GENERAL, VISCERAL, AND SPECIAL SENSORY (AFFERENT) PATHWAYS OF CRANIAL NERVES
Sensory pathways are composed of three major neurons: primary, secondary, and tertiary.
The primary sensory neuron cell bodies are usually located outside the central nervous system (CNS) in sensory ganglia. They are homologous with the dorsal root ganglia of the spinal cord but are usually smaller and are frequently overlooked;
The secondary sensory neuron cell bodies are located in the dorsal and lateral gray matter of the brain stem, and their axons usually cross the midline to project to the thalamus. The cell bodies that reside in the brain stem form the sensory group of cranial nerve nuclei;
The tertiary sensory neuron cell bodies are located in the thalamus, and their axons project to the sensory cortex.
The sensory component of the cranial nerves, except for cranial nerves (CNs) I and II, consists of the axons of the primary sensory neurons. CNs I and II are special cases that will be explained in the appropriate chapters. Because there are several modalities carried by sensory neurons, and because these modalities tend to follow different pathways in the brain stem, the loss experienced when sensory neurons are damaged depends, to a large extent, on the location of the lesion.Lesions in a peripheral nerve result in the loss of all sensation carried by that nerve from its field of distribution;
Sensory abnormalities resulting from lesions in the CNS depend on which sensory pathways are affected. For example, a lesion in the descending portion of the trigeminal nucleus results in loss of pain and temperature sensation on the affected side of the face but in little loss of discriminative touch, which is perceived in the middle and upper part of the same nucleus;
Damage to the thalamus results in a patchy hemianesthesia (numbness) and hemianalgesia (insensitivity to pain) on the contralateral (opposite) side of the body. There is often additional spontaneous pain of an unpleasant, disturbing nature on the partially anesthetized side.
SOMATIC, BRANCHIAL AND PARASYMPATHETIC MOTOR (EFFERENT) PATHWAYS OF CRANIAL NERVES
Voluntary motor pathways (somatic and branchial) are composed of two major neurons: the upper motor neuron and the lower motor neuron. The involuntary motor pathway (parasympathetic) is composed of three major neurons: the upper motor neuron, the lower motor neuron, and the tertiary motor neuron within a ganglion or body.
The upper motor neuron is usually located in the cerebral cortex. Its axon projects caudally through the corticobulbar tract† to contact the lower motor neuron in the brain stem. Most, but not all, of the motor pathways that terminate in the brain stem project bilaterally to contact lower motor neurons on both sides of the midline. Damage to any part of the upper motor neuron results in an upper motor neuron lesion (UMNL). The symptoms of an upper motor neuron lesion include:
Paresis (weakness) or paralysis when voluntary movement is attempted;
Increased muscle tone (spasticity);
Exaggerated tendon reflexes
Wasting of the muscles does not occur unless the paralysis is present for some time, at which point, some degree of disuse atrophy appears. These symptoms do not occur in those parts of the body that are bilaterally represented in the cortex. In the head and neck, all the muscles are bilaterally represented except the sternomastoid, the trapezius, those muscles below the eyebrow, and the tongue.
2. The lower motor neuron is located in the brain stem or upper cervical spinal cord. The cell bodies form the motor cranial nerve nuclei. Axons that leave these nuclei make up the motor component of the cranial nerves. Damage to any part of the lower motor neuron results in a lower motor neuron lesion (LMNL). The symptoms of a lower motor neuron lesion include:
Paresis (weakness) or, if all the motor neurons to a particular muscle group are affected, complete paralysis;
Loss of muscle tone (flaccidity);
Loss of tendon reflexes;
Rapid atrophy of the affected muscles;
Fasciculation (random twitching of small muscle groups)
The involuntary parasympathetic motor pathway differs from the voluntary somatic and branchial motor pathways in that it is a three-neuron chain. Its targets include smooth and cardiac muscle and secretory cells.
The upper motor neuron is located in a high cortical center. Axons project to parasympathetic nuclei in the brain stem;
The lower motor neuron is located in the brain stem nuclei and projects via CNs III, VII, IX, and X to ganglia located outside the CNS;
The tertiary neurons from these ganglia travel to their target cells in the head, thorax, and abdomen.